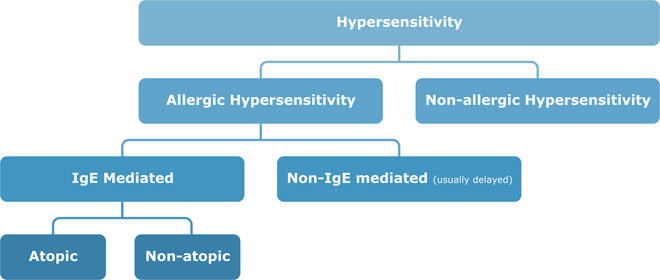
Allergic Hypersensitivity simply put, is an adverse exaggerated immune reaction to a protein (or allergen) in our environment, and which is normally harmless to the non-allergic person. Dr Adrian Morris explains…
An allergy may present as mild itching of the skin, tissue swelling and wheezing or even progress to full-blown life-threatening anaphylaxis, (anaphylactic shock) and death. Only a small proportion of the population exposed to an allergen will develop an allergic reaction. 18 million allergy sufferers live in the UK where 4% of the population also have a food allergy.
“Non-allergic” hypersensitivity reactions are those reproducible adverse reactions that do not involve the immune system (previously called intolerances). Diarrhoea triggered by lactose (cow’s milk sugar) intolerance is a good example of a non-allergic hypersensitivity (or food intolerance reaction).
Allergy develops after repeated exposure to the causative allergen and you don’t usually react on first exposure. Sensitisation takes place on initial exposure (a process that may take up to 6 weeks to develop) and no adverse reaction appears to occur during this sensitisation. Babies may be sensitised through their skin by their carers handling then after touching certain foods (peanuts). Some time later on repeated allergen exposure, the full-blown allergic reaction will occur. The tendency for some families to develop allergic sensitisation is termed Atopy.
During sensitisation, specific Immunoglobulin E (IgE) antibodies are produced by our white blood cells and on re-exposure these IgE antibodies bind the allergen and attach to Mast Cells or Basophils, which release Histamine and other immune molecules. This triggers the beginning of the Allergic Reaction, which may manifest with anything from a mild itch to anaphylaxis and death. Late phase (Non-IgE) reactions also may follow 6 to 24 hours later with Inflammation and tissue swelling.
Some people may become sensitised to an allergen and have positive allergy tests but not ever have an allergic reaction. This is called “Latent Allergy” and has no ill effects. These people go about their lives completely oblivious to the fact that they are sensitised.
Common Allergic Manifestations include Asthma, Allergic Rhinitis or Hay fever, Atopic Eczema, Contact Dermatitis, Urticaria or Hives, Food Allergy, Allergic Conjunctivitis, Wasp Venom Allergy and allergy to Medication such as Penicillin and Anaesthetics.
What constitutes a good allergy practitioner?
The Practitioner (doctor or nurse) needs to have plenty of time available for the consultation and a keen interest in allergy is paramount. In Allergology (the study of Allergy) the patient’s description of their allergy and careful questioning by the doctor goes 90% of the way to a correct diagnosis. This is usually followed by a brief examination of the relevant organs such as nose, eyes, lungs, glands and skin. Allergy tests should only be done to confirm the suspected allergy detected from the history. Tests should not be used as blind searches for an allergic component to the patient’s symptoms.
Once diagnosed, the patient needs to have the implications of their allergy explained to them in detail. They should be given some “easy to read” educational material to take home and digest. Understanding the nature and causes of the allergy will make future allergy control by the patient much more successful. A follow-up consultation is helpful as it provides an opportunity to discuss problems associated with the allergy and to reinforce the need for treatment.
What are those tell-tale signs that alert the doctor to probable allergy as the patient walks into the clinic?
- Allergic “shiners” are often a give-away – these are darkened areas of skin around the eye sockets, which are a result of increased blood congestion in the sinuses. They often resemble “Black Eyes” or look like “Mascara” around the eyes. There may be characteristic Dennie-Morgan infra-orbital folds or linear creases under the eyelids. The typical transverse nasal crease across the bridge of the nose is from constant nose itching and rubbing. The “allergic salute” is seen when the person’s hand constantly rubs the nose and is associated with facial grimacing or so called “Pulling of Faces” because the nose, eyes and ears are so itchy.
- After many years of Nasal Allergy, the sufferer develops a so-called “Long Faced” appearance with constant open-mouth breathing, nose blockage, a high arched palate and dental malocclusion with “Buck Teeth” often requiring Orthodontic treatment.
- The allergy sufferer’s skin has a dry and rough sandpaper-like texture on the outer arms which is called Keratosis Pilaris. In children, this is commonly associated with eczematous rashes on the face, in the elbow creases and behind the knees. In adults Eczema tends to affect other areas such as the neck, wrists and back of hands.
- The nose’s internal mucus membranes (called Turbinates) are usually swollen and oedematous with a pale blue appearance. The lower-eyelid conjunctival lining has a thickened “cobblestone” appearance and the eyes may be red, watery and itchy. Eye mucus is often white and “stringy”. Chronic middle ear mucus is called an Effusion or “Glue ear” often accompanies nasal allergies. Other common allergic manifestations are a wheezy chest, constant sneezing, itchy watery eyes and “Nettle ” rashes on the skin.
Case Histories to illustrate typical Allergy
Here are 3 short case histories to illustrate common allergy presentations:
First is Byron, a 5 year old who has a chronic dry rash, constant “cold” symptoms and an irritating cough at night.
He is an only child in a professional family, his mother smokes. There is a family history of asthma and hayfever. And he is unable to tolerate eggs.
On examination, he had typical allergic facial features with allergic rings around the eyes, Dennie Morgan folds under the eyes, a long face with mouth breathing and the nasal membranes were swollen. There was eczema on his legs and arms and his chest examination revealed slight wheezing.
We performed an exercise test and triggered asthma, which was reversed by inhaled salbutamol. He had inhalant Skin scratch tests and a food allergy screen. These showed Cat and egg allergy. His nasal cell smear showed sheets of allergy cells (Eosinophils). The Blood Count confirmed allergy (also Eosinophils) and the Chest xray revealed asthmatic lung hyperinflation changes – all confirming allergic asthma and allergic rhinitis with co-existent eczema and egg allergy.
By withdrawing egg from the diet and removing the cat from the home, symptoms dramatically improved. Now Byron only occasionally needs his reliever inhaler before sport or if he picks up the Common Cold or a viral illness. Byron is likely to outgrow his egg allergy by age 7 years.
Victoria is aged 13 years and she presents with a history of an acute adverse reaction to eating a nutty chocolate with itching swelling and collapse.
She had eaten chocolate before without any problems, but admitted to avoiding nuts as they made her feel “ill”. As a child she had vomited peanut butter and her mother had avoided peanuts and tree nuts in her diet ever since. On this occasion, she ate a chocolate bar in the cinema. Victoria noticed that he mouth immediately began to itch, her tongue and face became swollen, her throat began to constrict and she had an irritating cough. A “nettle” rash began to develop on her face and spread to her whole body, this was associated with a feeling of “dread” before she passed out. She was rushed to the local hospital A&E Department and injected with adrenaline, given antihistamines and hydrocortisone and luckily made a rapid recovery.
This illustrates how essential it is to identify the causative agent in the case of anaphylaxis – we tend to use RAST tests or skin prick tests for diagnosing allergy to nuts (one can be allergy to one individual nut only or many nuts). We did a nut mix food screen which was positive and on individual UniCAP RAST tests she had strong IgE reactions to Cashew nut and Peanut. We immediately referred her for dietetic advice on nut avoidance, and food label reading she had a Medic Alert bracelet issued, and carries an Epipen auto injector with a spare at home and school together with Piriton and Prednisilone tablets on hand.
Victoria has had no further reactions and now leads a full and happy life, knowing what to avoid. However she is unlikely to outgrow the nut allergy.
The final patient is Marion aged 27 years who presents to the allergy clinic with a 2 year history of fatigue, bloating, weight gain, dizziness and headaches.
She comes from a non-allergic family, and has no preceding history of asthma, hayfever or eczema. She had visited an alternative practitioner called a “Nutritionist” and had a VEGA Test, which involves measuring electric currents in the skin. As a result of this test she was told that she was allergic and intolerant to Yeast, Wheat Gluten and Sugar and put on a strict avoidance diet. The diet was very difficult to adhere to, as so many foods had to be avoided. Her symptoms had not improved and she presented to her Practice Nurse – asking if she was indeed allergic to these foods and what could be done to help.
We did a food skin test screen, which includes wheat, and this was negative. A specific skin test to Yeast was also negative. We confirmed this on blood testing. Her Total IgE level was in the low normal range. Sugar is not a common allergen as to be an allergen, there must be a protein component. Therefore there seemed to be no strong allergic trigger for her symptoms – we checked Marion’s thyroid function, which showed gross underactivity and Hypothyroidism.
Marion made a full symptom recovery after regular thyroxine supplementation. This highlights the need to consider alternative diagnoses to allergy even when the patient is convinced that they are allergic.
What should we do next? Who can help? Visit our appointments page for more information on allergy testing and treatments available. Find out where our clinics are located.
Written by Dr Adrian Morris
Reviewed 10th November 2025.
